OPINION: Unraveling the role of GIS in health disparities and equity
By Maria Assumpta Komugabe
Location matters: Understanding the influence of place on health
Where you live significantly influences your health outcomes and life expectancy. Up to 60% of your health is shaped by your surroundings, particularly your zip code/ neighborhood.
Factors such as socioeconomic status, community investment, and access to healthcare facilities play a pivotal role in shaping individual and community health, often outweighing personal behavior and clinical care.
Despite the common belief that more healthcare facilities lead to better health outcomes, true health lies in reduced reliance on medical intervention. Unfortunately, many low-income and rural areas lack adequate healthcare infrastructure, hindering community improvement efforts.
The environment consistently emerges as a primary determinant of health, highlighting the urgent need to address healthcare access disparities and invest in community development initiatives to foster healthier environments and improve overall health outcomes for everyone, irrespective of their zip code.
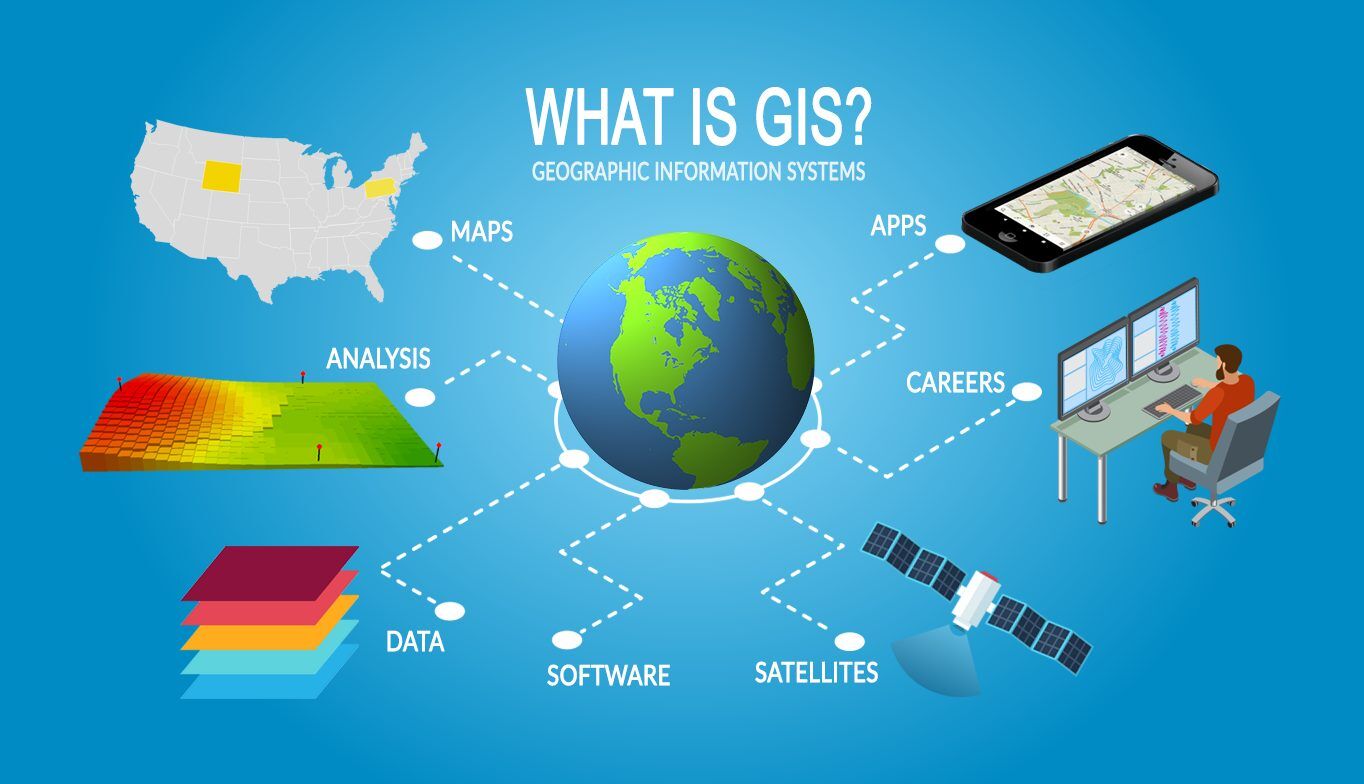
Leveraging GIS for health equity
In addressing the disparities in health outcomes related to one's place of residence, Geographic Information Systems (GIS) emerges as a powerful tool. GIS can analyze vast amounts of data to identify communities with disproportionate health challenges.
By integrating socio-economic data, health outcomes, and geographic information, GIS can pinpoint areas with limited access to healthcare facilities, inadequate infrastructure, and higher prevalence of chronic diseases. This analysis helps prioritize resources and interventions where they are most needed.
Optimizing healthcare resource allocation
GIS mapping enables healthcare planners to visualize spatial data and identify gaps in healthcare infrastructure. By overlaying demographic information and health indicators, GIS can predict future healthcare needs and optimize resource allocation.
Predictive modeling can forecast the demand for specific healthcare services in underserved areas, guiding decisions on the placement of clinics, hospitals, and mobile healthcare units.
Enhancing community engagement and outreach
GIS platforms facilitate community mapping exercises, empowering residents to identify local health priorities and participate in decision-making processes. Additionally, GIS-driven communication tools can personalize health education materials and outreach campaigns to resonate with diverse community groups.
Improving preventive care and early intervention
GIS spatial analysis can identify environmental hazards and social determinants of health that contribute to disease risk, informing public health policies and interventions to mitigate these risks.
Strengthening health surveillance and monitoring
GIS-based disease mapping allows for real-time monitoring of disease outbreaks, enabling rapid response and containment efforts. This information supports proactive public health measures, such as vaccination campaigns, vector control, and targeted health education initiatives.
In conclusion, GIS holds immense promise in addressing the complex interplay between place of residence and health outcomes.
By harnessing the power of spatial mapping and data analytics, stakeholders can develop evidence-based strategies to reduce health disparities, improve healthcare access, and promote community well-being. As we continue to advance GIS technologies and integrate them into public health practices, we can move closer to achieving health equity for all individuals, regardless of their zip code.